What is responsible for blood clotting? Blood clotting, also called coagulation, is a vital process that prevents excessive bleeding when blood vessels are injured. Without this essential mechanism, even a minor injury leads to serious blood loss and life-threatening complications. In this article, we will cover what is responsible for blood clotting, the key players involved in the process, and its importance in maintaining overall health.
What is blood clotting?
Blood clotting is the body’s natural response to an injury. It is a complex process that involves a series of chemical reactions and cellular activities aimed at stopping blood flow at the site of injury while maintaining circulation elsewhere. The primary goal of blood clotting is to form a stable clot that acts as a barrier to prevent further blood loss.
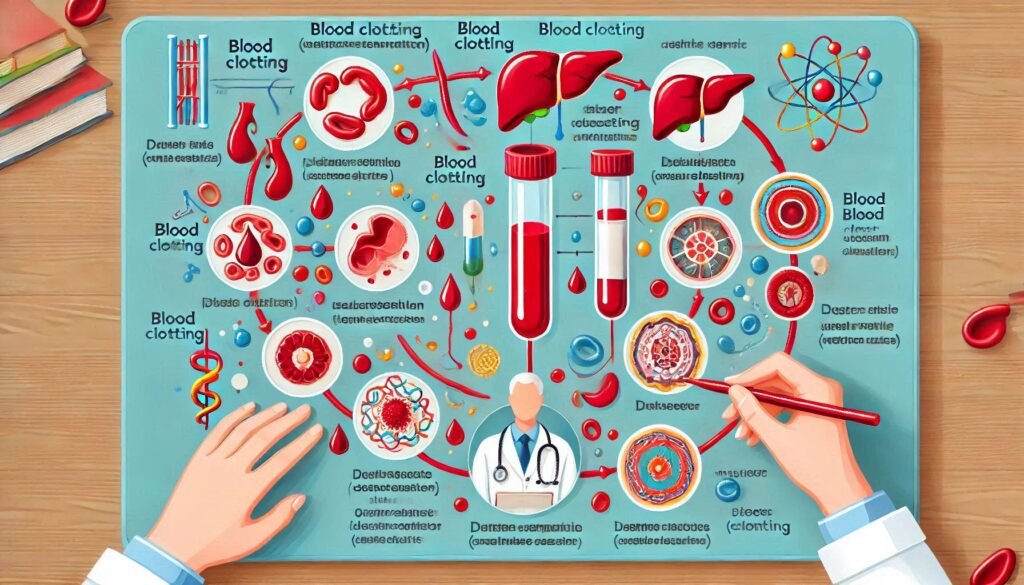
The Key Players in Blood Clotting
Several components work together to ensure efficient blood clotting. These include platelets, clotting factors, and blood vessels. Here’s a detailed look at each of these components:
1. Platelets
Platelets, also known as thrombocytes, are tiny, disk-shaped cells in the blood that play a crucial role in the clotting process. When a blood vessel is damaged, platelets are among the first responders. They adhere to the damaged site and release chemicals that attract more platelets, forming a temporary “platelet plug.”
- Normal platelet count: 150,000 to 450,000 per microliter of blood
- Key function: Formation of the primary plug to stop bleeding temporarily
2. Clotting Factors
Clotting factors are proteins in the blood that work in a sequential manner known as the clotting cascade. There are 13 primary clotting factors, labeled I through XIII. These factors work together to stabilize the platelet plug by forming a fibrin mesh.
- Example: Factor I (Fibrinogen) is converted to fibrin, creating a net-like structure that holds the clot together.
- Disorders: Deficiencies in clotting factors, such as hemophilia, can impair clot formation.
3. Blood Vessels
Blood vessels themselves play an active role in clotting. When damaged, they constrict (vasoconstriction) to reduce blood flow to the injured area. Additionally, the endothelial cells lining the vessels release signals that activate platelets and clotting factors.
How Does Blood Clotting Work? The Step-by-Step Process
The blood clotting process can be divided into three main stages:
1. Vascular Spasm (Vasoconstriction)
When a blood vessel is injured, it immediately constricts to reduce blood flow. This initial response helps limit blood loss and creates a favorable environment for the subsequent stages of clotting.
2. Formation of the Platelet Plug
Platelets adhere to the exposed collagen in the damaged blood vessel. They then release chemicals like ADP (adenosine diphosphate) and thromboxane A2, which recruit more platelets to the site. This aggregation forms a temporary plug.
3. Coagulation Cascade and Fibrin Formation
The clotting factors activate in a cascade-like manner, ultimately leading to the conversion of fibrinogen (Factor I) into fibrin. Fibrin forms a stable mesh that reinforces the platelet plug, creating a durable clot.
- Intrinsic Pathway: Activated by damage inside the blood vessel
- Extrinsic Pathway: Triggered by external trauma
- Common Pathway: Both pathways converge to form the final clot

Why is Blood Clotting Important?
Blood clotting serves several essential functions, including:
- Preventing Blood Loss: Clots stop bleeding at the site of injury, preventing excessive blood loss.
- Promoting Healing: The clot acts as a scaffold for tissue repair and wound healing.
- Protecting Against Infections: By sealing the wound, clots reduce the risk of bacteria and pathogens entering the bloodstream.
Disorders Related to Blood Clotting
While clotting is essential, abnormalities in this process can lead to serious health issues. These include:
1. Excessive Clotting (Hypercoagulation)
- Conditions: Deep vein thrombosis (DVT), pulmonary embolism
- Causes: Genetic disorders, prolonged immobility, obesity
- Risks: Clots can block blood flow to vital organs, causing complications like stroke or heart attack.
2. Impaired Clotting (Hypocoagulation)
- Conditions: Hemophilia, Von Willebrand disease
- Causes: Deficiency in clotting factors or platelets
- Risks: Increased bleeding risk, even from minor injuries
FAQs About Blood Clotting
Blood clotting is triggered by damage to blood vessels, which exposes collagen and other substances that activate platelets and clotting factors.
Vitamin K is critical for synthesizing several clotting factors, including Factor II (prothrombin). Deficiency in Vitamin K can impair clotting.
Common disorders include hemophilia, deep vein thrombosis, and disseminated intravascular coagulation (DIC).
Eating a balanced diet rich in Vitamin K (found in leafy greens) and maintaining healthy platelet levels can support clotting. Avoid smoking and manage conditions like diabetes.
Tests like Prothrombin Time (PT), Activated Partial Thromboplastin Time (aPTT), and Platelet Count assesses the clotting process.


Leave a Reply
You must be logged in to post a comment.